When it comes to medication adherence, a spoonful of simple makes the medicine go down.
Group Business Director James Langridge looks at why simple ideas are oftentimes ten times better than complex ones, in improving medical adherence.
We all know that the quality use of medicines depends on a patient’s adherence to their recommended treatments. We also know that in most categories up to 40% of patients can become non-compliant due to misunderstanding, forgetting, or deliberately ignoring healthcare advice. Not only does this have a negative impact on patient morbidity and mortality, but also on the healthcare system. Non-adherence across hypertension, dyslipidemia, and depression alone costs Australia $10.4 billion annually.
Though we may want to minimise non-adherence, tackling it can seem incredibly complex. Where do you start, what do you do, and what does ‘good’ look like? Whilst we certainly don’t have all the answers, we have developed a three-step guide to approaching non-compliance in a simple, but effective way.
Uncover the barriers to compliance.
There’s a wide variety of reasons for non-adherence, which will vary according to what patient group, disease area, and treatment you are focussing on. For example, a patient may decide that their treatment does not work, or that its side effects are too severe, or that they simply want to see if they can continue drug-free. Others may feel that a drug or administration method stigmatises them (as is the case with many people with schizophrenia, who refuse effective injectable treatments for that reason). With cases of unintentional non-adherence, a patient may not know (or may have forgotten) how to use the medicine or device correctly, or they may have been too embarrassed to ask their doctor the right questions and have no access to this information elsewhere.
The contextually sensitive nature of what drives non-adherence in different cases is why you will need to probe into the specific situation surrounding your patient, drug, and HCP interactions to understand that journey in full. What is it within this dynamic that would lead to the patient being uncertain about how to take the drug, or unwilling to follow guidance? Where and why does the carriage come off the tracks? A bit of market research, or even a few informal interviews with patients and HCPs will help uncover these insights.
Before jumping into Step Two, it’s really important to have spent some time getting to the heart of answering this first question, as the accuracy of your understanding of the problem will determine the effectiveness of the solutions you can come up with.
Ideate how to overcome those barriers.
Once you’ve identified the main reasons driving non-adherence, you can start to come up with potential solutions. For example, if the problem is around patient confusion, then a large part of the answer may lie in upskilling, training, and supporting the HCPs responsible for instructing the patient, so that they can do this more effectively and quickly. This could be via train-the-trainer masterclasses, webinars, leave pieces, training injection devices to use with the patients, or even providing a free helpline connecting patients with health experts for ongoing support. However, if the problem is more around the patient deciding to stop treatment, then this might lean more into how to better educate the patient around the need for drug adherence (even if they feel fine) and what to do in the event of side effects whilst remaining on treatment (and set up an easy process to facilitate them taking this action).
To help steer and validate your ideas, below is a list of commonly used interventions that have been proven to be successful adherence-enhancing strategies:
- Simplifying regimen characteristics: Adjusting timings, frequency and amount. Matching regimens to patients’ daily activities. Using adherence aids such as medication boxes and alarms
- Clearly imparting knowledge: Facilitating clear discussions between the patient and wider healthcare team. Providing clear written information (via print/ digital channels)
- Modifying patient beliefs: Ensure that patient understand the seriousness of the condition, risks of non-adherence, benefits of the treatment and has open channels to discuss any concerns easily
- Patient communication: Encourage and empower doctors to first listen more to patients and understand their feelings and concerns, and then implement shared decision making and ongoing follow up communications/ reminders
- Evaluating adherence: Enable doctors to accurately estimate, measure, and evaluate adherence reliably (via patient self-reports, pill counting, discussion guide to facilitate regular assessments)
You have your ideas, now make them simpler!
Now that you have your ideas, you need to pressure test them to ensure they will succeed in the real world. Importantly, your adherence program will not succeed if it is reliant on existing only in the most perfect of conditions. Instead, you should plan for the worst: time-poor healthcare professionals!
Here's what you need to do
1. Map out how your ideas work
2. Throw at them all the worst-case scenarios you can think of i.e.
- The doctors or nurses involved have no time and loads of other competing priorities
- The patient will forget everything and can follow only the simplest instructions
- Your internal team has only the smallest capacity to take on any issues/ additional workaround non-adherence
3. Refine your ideas so that they can succeed despite these worst-case scenarios
- What can you do to make your ideas even better, even simpler?
- How much of the patient training could you take off the plate of the doctors and nurses?
- Could you drive efficiencies in patient/ doctor connections and conversations?
- Could you automate responses to common patient inquiries?
- Can you make important patient information more visual or interactive? Could it be printed out easily by the patient to keep as a reminder in their wallet?
Thinking simpler in this way will not only ensure your ideas will effectively improve patient adherence, but it will also create a compelling differentiator for your brand that makes you stand out more with your prescribers, as you are making both their and their patients’ lives simpler — and who wouldn’t appreciate that?
Great medical adherence strategies, done simpler
FabriSol — A simple but innovative scratch-off adhesive sticker helping people to remember when and if they take their medication
Groove Health — App that uses a chatbot to help identify barriers to adherence, then alerts members of the patient’s care team on their dashboard, so they can follow up. Patients also receive specialised content and resources to address the potential barrier to adherence.
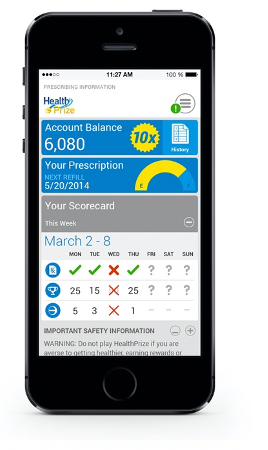
HealthPrize Technologies — An App where patients get points for reporting whether they took their medications; the points vary daily to keep it interesting. The company offers prizes such as gift cards for reaching certain levels, and patients can use points to earn health-related items or make charitable donations.